Search
Categories
- All
- Anesthesiology
- Breast Surgery
- Cancer Center
- Dermatology
- Ears, Nose, and Throat
- Emergency Room
- Endocrinology
- Family Medicine
- Fertility Clinic
- Gastroenterology
- General Surgery
- Gynecology
- Internal Medicine
- Laboratory
- Medical Imaging
- Nuclear Medicine
- Nutrition
- Obstetrics
- Ophthalmology
- Stomatology
- Orthopedics and Sports Medicine/Rehabilitation
- Pediatrics
- Pharmacy
- Psychology
- Respiratory Medicine
- Surgery
- Vasculocardiology
- PCR test (incl. bilingual report service fee)
Shingles
LEARN MOREWhat is shingles?
Shingles is a painful rash. Shingles is caused by the same virus that causes chickenpox (varicella-zoster). After you get chickenpox, the virus stays in your body for several years without causing any symptoms. Shingles occurs when the virus becomes active again. Once active, the virus will travel along a nerve to your skin and cause a rash.
What are the signs and symptoms of shingles?
Shingles often starts with pain in the back, chest, neck, or face. A rash then develops in the same area. The rash is usually found on only one side of the body. The rash may feel itchy or painful. It starts as red dots that become blisters filled with fluid. The blisters usually grow bigger, become filled with pus, and then crust over after a few days. You may also have any of the following:
• Fatigue and muscle weakness
• Pain when your skin is lightly touched
• Headache
• Fever
• Eye pain when exposed to light
What increases my risk for shingles?
• Age older than 50
• Exposure to the virus while your mother was pregnant with you
• A medical condition such as cancer, AIDS, or Hodgkin disease
• Treatment for cancer that decreases your immune system
• Stressful life events that weaken your immune system
• An organ or stem cell transplant
How is shingles diagnosed?
Your doctor will ask about your symptoms. Tell him if you have had chickenpox. Tell him if you have recently been around anyone who has chickenpox or shingles. The appearance of your rash will usually be enough for your doctor to know you have shingles. He may also send skin scrapingsor fluid from your blisters for tests.
How is shingles treated?
• Antiviral medicine helps decrease symptoms and healing time. It may also decrease your risk for nerve pain. You will need to start taking this medicine within 3 days of the start of symptoms to prevent nerve pain
• Pain medicine may be prescribed or suggested by your doctor. You may need NSAIDs, acetaminophen, or opioid medicine depending on how much pain you are in
• Topical anesthetics are used to numb the skin and decrease pain. They can be a cream, gel, spray, or patch
• Anticonvulsants decrease nerve pain and may help you sleep at night
• Antidepressants may be used to decrease nerve pain
• Epidural medicine is put into your spine to block pain. This medicine treats severe pain that does not get better with other pain medicines. Epidural medicine includes numbing medicine and steroids
Can I infect others?
The virus can be passed to a person who has never had chickenpox. This person may get chickenpox, but not shingles. You may pass the virus to others as long as you have a rash. The virus is spread by direct contact with the fluid from the blisters. Usually, you cannot spread the virus once the blisters dry up.
What are the risks of shingles?
If left untreated, shingles may cause eye problems, such as a drooping eyelid or blindness. It may lead to a brain infection or stroke. Shingles can also cause nerve damage and lead to twitching, dizziness, or loss of taste and hearing. The blisters may leave scars or changes in skin color. Shingles may cause pain even after the rash is gone. It may also lead to trouble moving parts of your body.
How can I care for myself?
Keep your rash clean and dry. Cover your rash with a bandage or clothing. Do not use bandages with adhesive. These may irritate your skin and make your rash last longer.
What can I do to help prevent shingles or a shingles outbreak?
A vaccine may be given to help prevent shingles. Ask for more information about this vaccine.
When should I seek immediate care?
• You have painful, red, warm skin around the blisters, or the blisters drain pus
• Your neck is stiff or you have trouble moving it
• You have trouble moving your arms, legs, or face
• You have a seizure
• You have weakness in an arm or leg
• You become confused, or have difficulty speaking
• You have dizziness, a severe headache, or hearing or vision loss
When should I contact my doctor?
• You feel weak or have a headache
• You have a cough, chills, or a fever
• You have abdominal pain or nausea, or you are vomiting
• Your rash becomes more itchy or painful
• Your rash spreads to other parts of your body
• Your pain worsens and does not go away even after you take medicine
• You have questions or concerns about your condition or care
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your caregivers to decide what care you want to receive. You always have the right to refuse treatment.
© 2017 Truven Health Analytics LLC All illustrations and images included in CareNotes® are the copyrighted property of A.D.A.M., Inc. or Truven Health Analytics.
Click the link for more information on Dermatology Clinical Service
Click the link for more information on Family Medicine Clinical Service
Tinnitus
LEARN MOREDo you hear a ringing, roaring, clicking, or hissing sound in your ears? Do you hear this sound often or all the time? Does the sound bother you a lot? If you answer yes to these questions, you may have tinnitus.
Tinnitus is a symptom associated with many forms of hearing loss. It can also be a symptom of other health problems.
What causes tinnitus?
• Hearing loss. People with different kinds of hearing loss also have tinnitus
• Loud noise. Too much exposure to loud noise can cause hearing loss and tinnitus
• Medicine. More than 200 medicines can cause tinnitus. If you have tinnitus and you take medicine, ask your doctor or pharmacist whether your medicine could be involved
• Wax or a foreign body in the ear canal
• Other health problems. Allergies, tumors, and problems in the heart and blood vessels, jaws, and neck can cause tinnitus
What should I do if I have tinnitus?
The most important thing you can do is to visit your doctor. Your doctor will try to find out what is causing your tinnitus. He or she can check your hearing and examine your ears to see if the canals are obstructed by wax. Your doctor will also check to see if it is related to blood pressure, kidney function, diet, or allergies. Be sure to bring a list of all your medications and dietary supplements so your doctor can determine whether your tinnitus is related to any medicine you are taking.
To learn more about what is causing your tinnitus, your doctor may refer you to an otolaryngologist, an ear, nose, and throat doctor. He or she will examine your ears and your hearing to try to find out why you have tinnitus. Another hearing professional, an audiologist, can measure your hearing. If you need a hearing aid, an audiologist can fit you with one that meets your needs.
How will the doctor treat my tinnitus?
Although there is no cure for tinnitus, several treatments may give you some relief. Not every treatment works for everyone, so you may need to try several to find the ones that help.
Treatments can include:
• Hearing aids. Many people with tinnitus also have a hearing loss. Wearing a hearing aid makes it easier for some people to hear the sounds they need to hear by making them louder. The better you hear other people talking or the music you like, the less you notice your tinnitus
• Maskers. Maskers are small electronic devices that use sound to make tinnitus less noticeable. Maskers do not make tinnitus go away, but they make the ringing or roaring seem softer. Some people find that maskers hide their tinnitus well enough that they can barely hear it. Some people sleep better when they use maskers. Listening to static at a low volume on the radio or using bedside maskers can help. These are devices you can put by your bed instead of behind your ear. They can help you ignore your tinnitus and fall asleep
• Medicine. Some medicines may ease tinnitus. If your doctor prescribes medicine to treat your tinnitus, he or she can tell you whether the medicine has any side effects
• Cognitive therapy. This treatment uses a combination of counseling and maskers. The therapist can help you learn how to deal with your tinnitus better. You may also use maskers to make your tinnitus less noticeable. After a while, some people learn how to avoid thinking about their tinnitus. It takes time for this treatment to work, but it can be very helpful
• Counseling. People with tinnitus may become depressed. Talking with a counselor or people in tinnitus support groups may be helpful
What can I do to help myself?
• If you wear hearing aids, be sure they fit well
• See an otologist (hearing specialist)
• Tinnitus support groups are available online
• Find out more about music therapy for tinnitus
• Acupuncture may be helpful
• Try relaxation techniques, mindfulness and breathing exercises
• Consult a psychologist or neuropsychiatrist
• Consider a white noise generator
• Cognitive behavioral therapy may help
Think about things that will help you cope. Many people find listening to music very helpful. Focusing on music might help you forget about your tinnitus for a while. It can also help mask the sound. Other people like to listen to recorded nature sounds, like ocean waves, the wind, or even crickets.
Avoid anything that can make your tinnitus worse. This includes smoking, alcohol, and loud noise. If you are a construction worker, an airport worker, or a hunter, or if you are regularly exposed to loud noise at home or at work, wear ear plugs or special earmuffs to protect your hearing and keep your tinnitus from getting worse.
If it is hard for you to hear over your tinnitus, ask your friends and family to face you when they talk so you can see their faces. Seeing their expressions may help you understand them better. Ask people to speak louder, but not shout. Also, tell them they do not have to talk slowly, just more clearly.
This document is intended to provide health related information so that you may be better informed. It is not a substitute for your care team's medical advice and should not be relied upon for treatment for specific medical conditions.
© 2017 The General Hospital Corporation.
Primary Care Office lnSite
developed by the MGH Laboratory of Computer Science and Division of General Internal Medicine
Click the link for more information on E.N.T Clinical Service
Gastritis
LEARN MOREWhat is gastritis?
Gastritis is inflammation or irritation of the lining of your stomach.
What increases my risk for gastritis?
• Infection with bacteria, a virus, or a parasite
• NSAIDs, aspirin, or steroid medicine
• Use of tobacco products or alcohol
• Trauma such as an injury to your stomach or intestine
• Autoimmune disorders such as diabetes, thyroid disease, or Crohn disease
• Stress
• Age older than 60 years
• Illegal drugs, such as cocaine
What are the signs and symptoms of gastritis?
• Stomach pain, burning, or tenderness when you press on it
• Stomach fullness or tightness
• Nausea or vomiting
• Loss of appetite, or feeling full quickly when you eat
• Bad breath
• Fatigue or feeling more tired than usual
• Heartburn
How is gastritis diagnosed?
Your doctor will ask about your signs and symptoms and examine you. You may need any of the following:
• Blood tests may be used to show an infection, dehydration, or anemia (low red blood cell levels)
• A bowel movement sample may be tested for blood or the germ that may be causing your gastritis
• A breath test may show if H pyloriis causing your gastritis. You will be given a liquid to drink. Then you will breathe into a bag. Your doctor will measure the amount of carbon dioxide in your breath. Extra amounts of carbon dioxide may mean you have an H pylori infection
• An endoscopy may be used to look for irritation or bleeding in your stomach. Your doctor will use an endoscope (tube with a light and camera on the end) during the procedure. He or she may take a sample from your stomach to be tested
How is gastritis treated?
Your symptoms may go away without treatment. Treatment will depend on what is causing your gastritis. Your doctor may recommend changes to the medicines you take. Medicines may be given to help treat a bacterial infection or decrease stomach acid.
How can I manage or prevent gastritis?
• Do not smoke. Nicotine and other chemicals in cigarettes and cigars can make your symptoms worse and cause lung damage. Ask your doctor for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your doctor before you use these products
• Do not drink alcohol. Alcohol can prevent healing and make your gastritis worse. Talk to your doctor if you need help to stop drinking
• Do not take NSAIDs or aspirin unless directed. These and similar medicines can cause irritation of your stomach lining. If your doctor says it is okay to take NSAIDs, take them with food
• Do not eat foods that cause irritation. Foods such as oranges and salsa can cause burning or pain. Eat a variety of healthy foods. Examples include fruits (not citrus), vegetables, low-fat dairy products, beans, whole-grain breads, and lean meats and fish. Try to eat small meals, and drink water with your meals. Do not eat for at least 3 hours before you go to bed
• Find ways to relax and decrease stress. Stress can increase stomach acid and make gastritis worse. Activities such as yoga, meditation, or listening to music can help you relax. Spend time with friends, or do things you enjoy
Call 120 for any of the following:
• You develop chest pain or shortness of breath
When should I seek immediate care?
• You vomit blood
• You have black or bloody bowel movements
• You have severe stomach or back pain
When should I contact my doctor?
• You have a fever
• You have new or worsening symptoms, even after treatment
• You have questions or concerns about your condition or care
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your caregivers to decide what care you want to receive. You always have the right to refuse treatment.
© 2017 Truven Health Analytics LLC All illustrations and images included in CareNotes® are the copyrighted property of A.D.A.M., Inc. or Truven Health Analytics.
Click the link for more information on Gastroenterology Clinical Service
A Beautiful Butterfly That Keeps You Healthy
LEARN MOREThe thyroid gland is a butterfly-shaped endocrine gland that is normally located in the lower front of the neck. The thyroid's job is to make thyroid hormones, which are secreted into the blood and then carried to every tissue in the body. Thyroid hormone helps the body use energy, stay warm and keep the brain, heart, muscles, and other organs working as they should.
Hyperthyroidism
The term hyperthyroidism refers to any condition in which there is too much thyroid hormone produced in the body. In other words, the thyroid gland is overactive.
What are the symptoms of hyperthyroidism?
Since hyperthyroidism increases your metabolism, every function of the body tends to speed up:
• Nervousness, irritability, increased sweating, heart racing, hand tremors, anxiety, difficulty sleeping, tired is very common
• Thinning of the skin, fine brittle hair and weakness in muscles, especially in the upper arms and thighs
• More frequent bowel movements, but diarrhea is uncommon
• Lose weight despite a good appetite
• For women, menstrual flow may lighten and menstrual periods may occur less often
• Enlarged eyes and swelling of the front of the neck
What causes hyperthyroidism?
The most common causes include Graves disease (GD), toxic multinodular goiter, toxic adenoma and painless thyroiditis.
How is hyperthyroidism diagnosed?
• Indicated symptoms and physical examinations
• Confirm by laboratory tests that measure the amount of thyroid hormones
• Measure levels of thyroid autoantibodies
• Imaging of thyroid glands
How is hyperthyroidism treated?
Hyperthyroidism can be effectively cured by anti-thyroid drugs, oral radioactive iodine capsule or surgical removal of all or most of thyroid gland. However, no single treatment is be st for all patients with hyperthyroidism. The appropriate choice of treatment will be influenced by the patient's age, the type of hyperthyroidism, the severity of hyperthyroidism, other medical conditions that may affect the problems, and the patient's own preference. It may be a good idea to consult with an endocrinologist who is experienced in the treatment of hyperthyroid patients.
Are other family members at risk?
Because hyperthyroidism, especially Graves' disease, may run in families, examinations of the members of your family may reveal other individuals with thyroid problems.
Hypothyroidism
Hypothyroidism (underactive) is an underactive thyroid gland. Hypothyroidism means that the thyroid gland can't make enough thyroid hormone to keep the body running normally. People are hypothyroid if they have too little thyroid hormone in the blood. Common causes are autoimmune disease (Hashimoto's thyroiditis), surgical removal of the thyroid, and radiation treatment.
What are the symptoms of hypothyroidism?
When thyroid hormone levels are too low, the body's cells can't get enough thyroid hormone and the body's processes start slowing down. As the body slows, you may notice that you feel colder, you tire more easily, your skin is getting drier, you're becoming forgetful and depressed, and you've started getting constipated. Because the symptoms are so variable and nonspecific, the only way to know for sure whether you have hypothyroidism is with a simple blood test for TSH.
Keeping other people informed:
• Tell your hypothyroidism to your relatives and encourage them to get periodic TSH tests
• Tell your other doctors and your pharmacist about your hypothyroidism and the drug and dose with which it is being treated
• If you start seeing a new doctor, tell the doctor that you have hypothyroidism and you need your TSH tested every year
• If you are seeing an endocrinologist, ask that copies of your reports be sent to your primary care doctor
What can you expect over the long term?
• There is no cure for hypothyroidism, and most patients have it for life. There are exceptions: many patients with viral thyroiditis have their thyroid function return to normal, as do some patients with thyroiditis after pregnancy
• Hypothyroidism may become more or less severe, and your dose of thyroxine may need to change over time. You have to make a lifetime commitment to treatment. But if you take your pills every day and work with your doctor to get and keep your thyroxine dose right, you should be able to keep your hypothyroidism well controlled throughout your life
• Your symptoms should disappear and the serious effects of low thyroid hormone should improve. If you keep your hypothyroidism well-controlled, it will not shorten your life span
What causes hypothyroidism?
There can be many reasons why the cells in the thyroid gland can't make enough thyroid hormone. Here are the major causes, from the most to the least common:
• Autoimmune disease
• Surgical removal of part or all of the thyroid gland
• Radiation treatment
• Congenital hypothyroidism (hypothyroidism that a baby is born with)
• Thyroiditis
• Medicines which prevent the thyroid gland from being able to make hormones
• Too much or too little iodine
• Damage to the pituitary gland
• Rare disorders that infiltrate the thyroid
Thyroid Nodules
Thyroid nodules refer to an abnormal growth of thyroid cells that forms a lump within the thyroid gland. Although the vast majority of thyroid nodules are benign (noncancerous), a small proportion of thyroid nodules do contain thyroid cancer. In order to diagnose and treat thyroid cancer at the earliest stage, most thyroid nodules need some type of evaluation.
What are the symptoms of thyroid nodules?
The important points to remember are the following:
• Thyroid nodules generally do not cause symptoms and mostly discovered incidentally
• Thyroid function tests are very important, especially when you have symptoms
• Thyroid function tests are most typically normal - even when cancer is present in a nodule
• To determine a thyroid nodule is to make sure your doctor checks your neck
What causes thyroid nodules and how common are they?
The causes of most thyroid nodules is unknown even though they are extremely common. Fortunately, over 90% of such nodules are benign. Hashimoto's thyroiditis, which is the most common cause of hypothyroidism, is associated with an increased risk of thyroid nodules. Iodine deficiency or overload is also known to cause thyroid nodules.
How is a thyroid nodule evaluated and diagnosed?
• Once the nodule is discovered, your doctor will try to determine whether the rest of your thyroid is healthy or whether the entire thyroid gland has been affected by a more general condition such as hyperthyroidism or hypothyroidism. Your physician will feel the thyroid to see whether the entire gland is enlarged and whether a single or multiple nodules are present
• Since it's usually not possible to determine whether a thyroid nodule is cancerous by physical examination and blood tests alone, the evaluation of the thyroid nodules often includes specialized tests such as thyroid ultrasonography and fine needle biopsy. Thyroid ultrasound is a key tool and a painless test to obtain a picture of the thyroid and evaluate thyroid nodules
• A fine needle biopsy of a thyroid nodule may sound frightening, but the needle used is very small and a local anesthetic may not even be necessary. For a fine needle biopsy, your doctor will use a very thin needle to withdraw cells from the thyroid nodule. The biopsy does not usually require any other special preparation (no fasting) and the patients typically return home or to work after the biopsy without even needing a bandaid
How are thyroid nodules treated?
• All thyroid nodules that are found to contain a thyroid cancer or highly suspected should be removed by an experienced thyroid surgeon
• Most thyroid cancers are curable and rarely cause life-threatening problems
• Thyroid nodules that are benign by FNA or too small to biopsy should still be watched closely with ultrasound examination every 6 to 12 months and annual physical examination by your doctor
Fine Needle Aspiration (FNA) Biopsy of Thyroid Nodules
A fine needle aspiration (FNA) biopsy of a thyroid nodule is a simple and safe procedure. Typically, the biopsy is performed under ultrasound guidance to ensure accurate placement of the needle within the thyroid nodule. You will be asked to lie down on your back with your head tipped backwards, so that your neck is extended. Sometimes, a pillow is placed under your shoulders to help you get in right position for the biopsy.
During the procedure you may feel some neck pressure from the ultrasound probe and from the needle. You will be asked to remain as still as possible and avoid coughing, talking and swallowing during the biopsy.
How can you prepare for your thyroid FNA?
• Most medications can be continued. However, anticoagulant often need to be stopped temporarily in anticipation of your thyroid biopsy for the increasing risk of bleeding caused by these drugs. It is common to receive specific instructions regarding when to stop taking medications from your doctor's office prior to the procedure
• Generally, you will not be required to be fasting on the day of your appointment
• During the thyroid biopsy, ultrasound gel will be applied to the neck to obtain ultrasound images. This gel is water soluble and non-toxic, but may get on clothing or jewelry. You may wish to wear comfortable clothing and take off any jewelry from around the neck for the procedure
How is a thyroid FNA performed?
• The neck will first be cleaned with an antiseptic. A local or topical anesthetic may be applied. For the biopsy, your doctor will use a very thin needle to withdraw cells from the thyroid nodule. The needle used is smaller in diameter than those used in most blood draws. Your doctor will insert the needle through the skin and into the thyroid nodule. After the sampling, which only takes several seconds, the needle will be removed. New needles are used for additional samples. Several samples of cells will be obtained, by sticking a fine needle in various parts of the nodule usually between two and six times. This assures a better chance to find cancerous cells if they are present
• If there is fluid in the nodule, a syringe may be used to drain it
• Once the biopsy is completed, pressure will be applied to the neck. The procedure usually lasts less than 30 minutes
What should you expect after the procedure?
• The procedure is usually performed using a local anesthetic and no medications are used that affect consciousness or thinking. After the procedure, you may be asked to sit up slowly to prevent you from getting lightheaded. Most patients typically leave feeling well. Because of this, it is not generally necessary to bring a companion to help or drive you home
• Some neck discomfort at the site of the biopsy is expected following the procedure. Pain killer and ice compresses can be used to relieve discomfort
What happens to the biopsy material after the procedure?
The biopsy samples may be used to make slides immediately and/or collected in a solution to wash excess blood. Specially trained doctors, cytopathologists, then make slides from the material and examine them under a microscope to make a diagnosis.
How long does it take for the results to return?
Generally, it can take anywhere from 3-4 working days for the result to return.
With reference to the website of the American Thyroid Association:
https://www.thyroid.org/hyperthyroidism
https://www.thyroid.org/hypothyroidism
https://www.thyroid.org/thyroid-nodules
https://www.thyroid.org/fna-thyroid-nodules
Click the link for more information on Thyroid Clinic Clinical Service
Bronchoscopy Examination
LEARN MOREWhat is a bronchoscopy?
A bronchoscopy is a procedure where a tube is inserted into the lower respiratory tract via the nose or mouth. This allows your physician to clearly visualize lesions in the trachea and bronchi. The bronchoscope is equipped to take samples of tissue directly observed by your physician for biopsy, to take smears by brushing, and to perform bronchial lavage. The equipment involved allows your physician to make an accurate diagnosis and to perform treatment more easily.
The bronchoscope is a soft and flexible tube with a small diameter, enabling a clear field of vision with a high degree of safety. The patient experiences minimal discomfort and only requires a local anesthetic. Most importantly, a bronchoscopy is the best method for diagnosing bronchial lesions. It can be used to discover lesions deep within the trachea, bronchi, and lungs that are difficult to detect that would not be found using chest CT. Diagnosis and treatment can be performed without the need to perform surgery.
When does a bronchoscopy need to be performed?
A bronchoscopy is needed to diagnose disease in the following circumstances:
• Causes of chronic cough,hemoptysis or blood-stained sputum,localized wheezing or hoarseness are unknown
• Chest X-ray and/or CT suggests abnormal changes
• Evaluation before thoracic operation
• Diagnosis for laceration or rupture of the trachea or bronchi in chest trauma
• Etiological diagnosis of infectious disease of the lung or bronchi
• Management of the airways during mechanical ventilation
• Diagnosis and treatment for fistulas of the trachea or bronchi
A bronchoscopy is needed for disease treatment in the following circumstance:
• Remove foreign objects from the bronchi, clearing abnormal secretions from the trachea, such as sputum, pus, and blood clots
• Remove emboli from the bronchi and pulmonary reexpansion in the event of pulmonary atelectasis caused by embolism involving pus, sputum, or blood
• Confirm the location of bleeding for patients with hemoptysis, then attempting to stop bleeding locally.
• Perform local radiation or local injection with chemotherapy drugs for patients with lung cancer
• Guided intubation of the airways and guided bronchial intubation where there are difficulties with intubation
• Laser, microwave, frozen, or high-frequency electrosurgical treatment for patients with benign or malignant tumors of the airways
When should a bronchoscopy not be performed?
• Active massive hemoptysis
• Severe arrhythmia
• Recent myocardial infarction or history of unstable angina pectoris
• Severe heart or pulmonary dysfunction
• Thrombocytopenia, coagulation dysfunction or the other bleeding disorder.
• Newly onset cerebral infarction or hemorrhage
• Aortic aneurysm
• Incompatibility or intolerable to bronchoscopy exam
What should I pay special attention to before my bronchoscopy?
• Before the bronchoscopy do not eat or drink for 4–6 hours,sign the consent form and a family member should accompany you on the day of the procedure
• Before the bronchoscopy give an accurate account of your health condition and past medical history to your physician. Remember to also let your physician know about any drug allergies, anticoagulants orantiplatelet drugs still used, hypertrophic rhinosinusitis, snoring, throat surgery you have had done, or serious cervical vertebrae diseases you may have
• Before the bronchoscopy take medications for illnesses strictly following the schedule provided by your physician. For example, medications for hypertension or heart disease can be taken orally two hours before the bronchoscopy and will not affect the procedure
• Before the bronchoscopy complete your preoperative examination: This includes chest CT, ECG, FBC, check for infections pre-surgery, and blood coagulation studies. Before leaving home, be sure to bring any chest X-ray or CT images, ECG, FBC, and blood coagulation reports for your physician to look at
• After the bronchoscopy wait outside the examination room after your procedure for at least 30 minutes to ensure that you are not experiencing any dizziness or other symptoms before you leave the hospital
• After the bronchoscopy appearance of blood-stained sputum following bronchoscopy is normal. See your doctor immediately if there is a significant amount of hemoptysis, bloody sputum, intense chest pain, difficulty breathing, recurring fevers, or arrhythmia
• After the bronchoscopy rest well and avoid talking to reduce hoarseness and a painful throat or chest
• After the bronchoscopy do not eat or drink for 2–3 hours following the procedure. Try drinking some warm water 3 or more hours after the procedure. If you are not choking or coughing, you can eat some cool, mild food
Is a bronchoscopy dangerous?
A bronchoscopy is a relatively safe procedure. Complications may occur (such as allergies to anesthetics, laryngeal edema, cramps in the airways, hypoxia, infections, bleeding, pneumothorax, and cardiocerebral events), however the chance of them occurring is low, and your physician will actively respond if such events occur. Your physician will perform strict checks, especially before the procedure, for indications and contraindications, to ensure that you are prepared. During the procedure, your physician will perform close monitoring, and respond immediately to any symptoms, reducing the risk of complications, and ensuring that the procedure is safe and effective.
Why is fluorescence bronchoscopy necessary?
Autofluorescence bronchoscopy (AFB) is a new type of bronchoscopy procedure combining regular white light bronchoscopy (WLB) with cell autofluorescence and information technology. This equipment stimulates cell fluorescence, to determine differences in cell fluorescence. The principle behind it is that dysplasia and microinvasive carcinoma of the bronchial epithelium occurs during blue laser exposure creates a weaker red fluorescence and weaker green fluorescence compared with normal tissue. This makes lesions appear in a reddish brown color whereas normal tissue appears green. Computer-aided imaging techniques enable such lesions and their extent to be identified. AFB is unique compared with other microscopic techniques, as it allows discovery of extremely minute lesions, therefore increasing the sensitivity and accuracy of biopsies carried out via bronchoscopy.
As with regular bronchoscopies, AFB is suitable for screening and diagnosis for patients at high risk of developing lung cancer and central type lung cancer in its early stages: AFB is also suitable as a preoperative examination or follow-up examination for lung cancer, useful in determining the scope of surgery prior to a procedure, avoiding resection line involvement, and in the early discovery of relapse and local metastasis following surgery.
Reference
中华医学会呼吸病学分会:诊断性可弯曲支气管镜应用指南(2008年版)
Click the link for more information on Respiratory Medicine Clinical Service
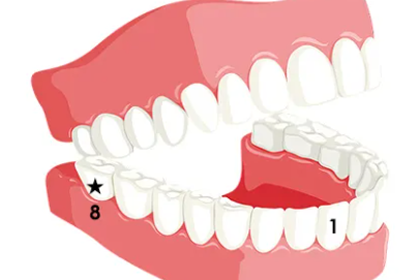
How to extract wisdom teeth? What should I pay attention to after wisdom teeth?
LEARN MOREN/A
Do wisdom teeth have to be removed? How to judge whether there are wisdom teeth?
LEARN MOREN/A

How to treat allergic rhinitis?
LEARN MOREN/A

What is allergic rhinitis? What are the symptoms of allergic rhinitis?
LEARN MOREN/A

How to prevent osteoporosis? Precautions for Osteoporosis Exercise
LEARN MOREN/A
- First page
- Previous page
- ...
- 21
- 22
- 23
- 24
- 25
- ...
- Next page
- Last page








